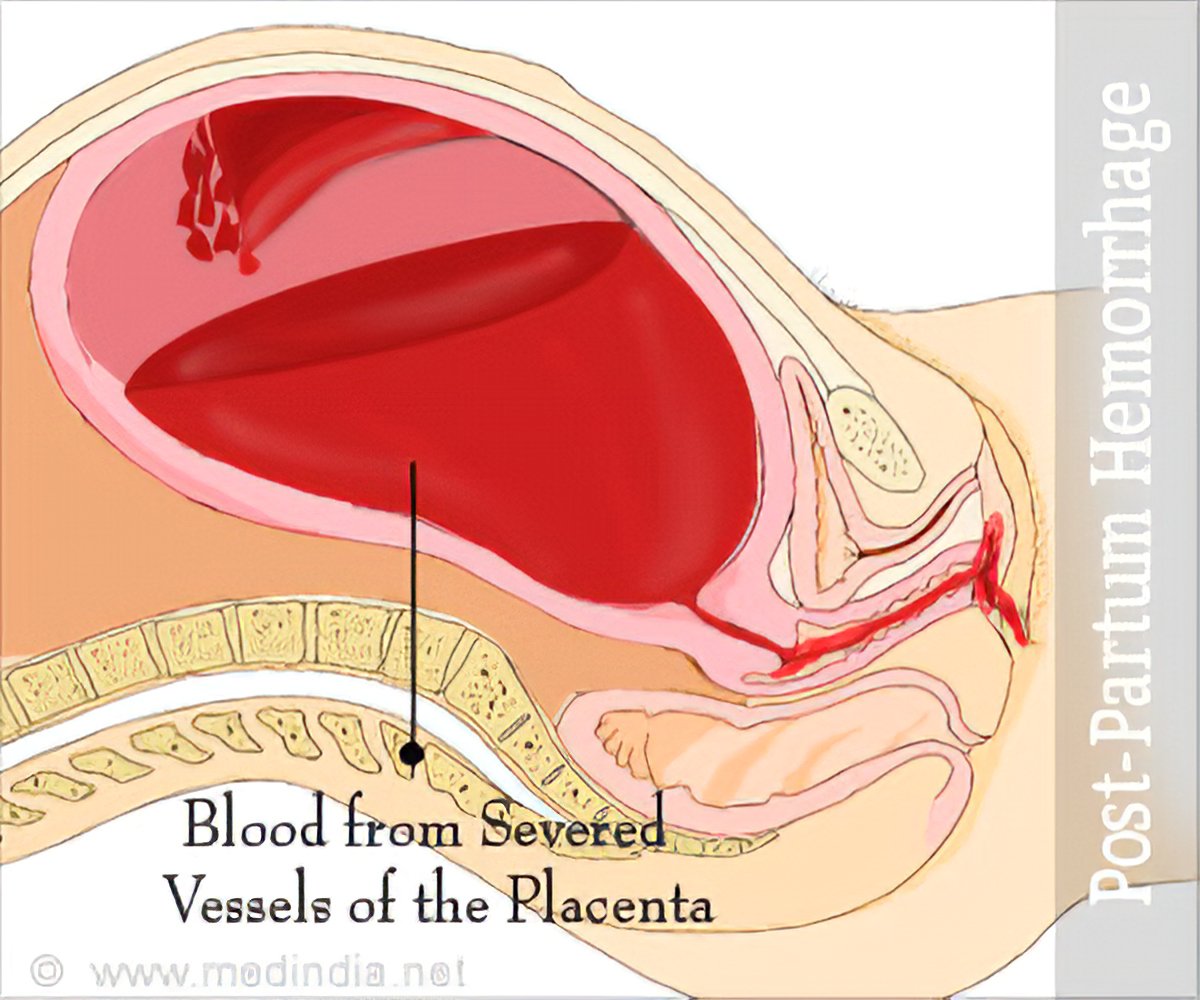
Definition: Postpartum haemorrhage is bleeding from the genital tract during the 3rd stage of labour, or within 24 hours after delivery of the placenta to the amount of 500mls or any amount that could change the patient’s condition. It is responsible for most maternal deaths. Shock sets in more quickly and can be irreversible. Anaemia is a predisposing factor, if it occurs within 24 hours of delivery, it’s termed primary postpartum haemorrhage and secondary postpartum haemorrhage if it occurs after 24 hours of delivery.
Causes of Primary PPH
- Retained placenta.
- Retained cotyledon.
- Genital trauma.
- Disseminated intramuscular uterus (DIC).
- Inversion of the uterus.
Cause of Secondary PPH
- Chorioamniolitis
- Retained products
Management
Basically, PPH is manage on three principles.
- Call an obstetrician.
- Stop the bleeding.
- Resuscitate the mother.
- Massage the uterus to stimulate contraction and expel the placenta if possible.
- Stay with your patient and shout for help
- Give ergometrine 0.5mls I.V and put up a drip.
- Empty bladder
- If placenta is already expelled, expel clots. Try to expel clot with the contraction caused by the ergometrine but if she is still bleeding severely, use manual removal to save the patient.
Types of PPH
Atonic postpartum haemorrhage
This is bleeding from the placental site when the uterus is not well contracted. This is a failure of a myometrium at the placental site to contract and retract and to compress torn blood vessels and control blood loss by a living ligature action.
Cause
- Incomplete separation of placenta.
- Retained cotyledon, placental fragments or membranes.
- Prolonged labour and obstructed labour resulting in uterine inertia.
- Rapid expulsion of large body.
- Poly hydraminous, multiple pregnancy that over stretches the uterus
- Adherent placenter that has partially separated.
- Precipitate labour.
- Mismanagement of the ill state of labour.
- Prolonged anaesthesia.
- Fibroids.
Management of Atonic PPH
- Ask the mother to empty her bladder
- Ask the mother to breastfeed the baby
- Massage the uterus
- Empty the uterus
- Bimanual compression; this can be done externally or internally by placing one hand on the fundus and the other above the symphysis pubis (external) or in anterior fornix (internally) and squeeze until clotting occurs usually clotting takes place 7-10 minutes later. Remove the external hand to check whether the bleeding has stopped or not. The dangers of this methods are further haemorrhage, shock or infection.
Traumatic postpartum haemorrhage
This is bleeding from a laceration of the cervix, vaginal wall and perineum episiotomy or even from ruptured uterus.
Cause
- Delivery through partially dilated cervix
- Instrumental delivery which causes bruises.
- Difficult delivery such as face to pubis.
Management of traumatic PPH
When bleeding is due to tear, explore the area for the tear, clamp the bleeding point and suture. Make sure that the uterus is not ruptured. If the laceration is sutured and bleeding stops, make sure that the uterus is well contracted. If bleeding is from bruised cervix place a pack against it for a few minutes to an hour. If you do this, leave catheter in situ.
If bleeding is from ruptured uterus, transfer to a hospital as soon as possible; go with the patient will full written report stating date, and time of departure.
Hypofibrinogenaemia
This is bleeding due to a clotting defect where the patient continues to bleed despite treatment for the other types of postpartum haemorrhage.
Causes
- Placental abruption.
- Intrauterine death which is prolonged.
- Amniotic fluid embolism.
- Preeclampsia, Eclampsia.
- Hepatitis.
Management of hypofibrinogenaemia (DIC)
- Fresh blood transfusion.
- Fibrinogen or triple strength plasma transfusion.
- Serve prescribed medication.
The patient’s response to treatment depends on how early it is initiated hence seek medical attention as soon as possible. Advice Hospital delivery for the next time and instruct her to explain to the doctor or nurse.
Consequences of PPH
- Shock and collapse which could result in death.
- Puerperal anaemia.
- Fear of further pregnancy.
- Sheehan’s syndrome which is due to anterior pituitary necrosis.
- Infection.
Prevention of PPH
Good Antenatal Care
- Accurate history taking to find out if she had PPH in previous delivery.
- Use hemoglobin to treat anaemia. Book high risk for hospital delivery.
- Try and prevent prolonged or obstructed labour.
- Make sure that the mother rests as much as possible during 1st stage and prevent dehydration.
- Keep bladder empty.
- Deliver the head slowly and control it.
- Active management of third stage labour.
Read Also
Pregnancy Induced Hypertension (PIH)Abortion
Ectopic Pregnancy
Antepartum Haemorrhage






3 Comments
Thanks very much 🙏
ReplyDeleteVery educative
ReplyDeleteNow, by you doing this course, you would not only have enhanced your subject matter knowledge, but the chances of you getting noticed by the best healthcare settings also increase. Violence prevention training
ReplyDelete