The term spontaneous abortion, which has a negative connotation to many patients, is gradually being replaced by the word miscarriage. Both terms original defined pregnancy losses prior to 20 weeks gestation, but they are more commonly used by physicians to describe first trimester losses. The pre-embrayonic period is defined as conception through the first 5 weeks of pregnancy from the first day of the last menstrual period. The embrayonic period encompasses 6 to 9 weeks gestation, and the fetal period is from 10 weeks until delivery.
Miscarriages are the most common complication of pregnancy, with an overall incidence of approximately 15% among clinically recognized pregnancies. The rate of miscarriage is heavily dependent upon the past obstetric history, being higher among women with prior miscarriages and lower among women whose pregnancy(ies) ended in live births.
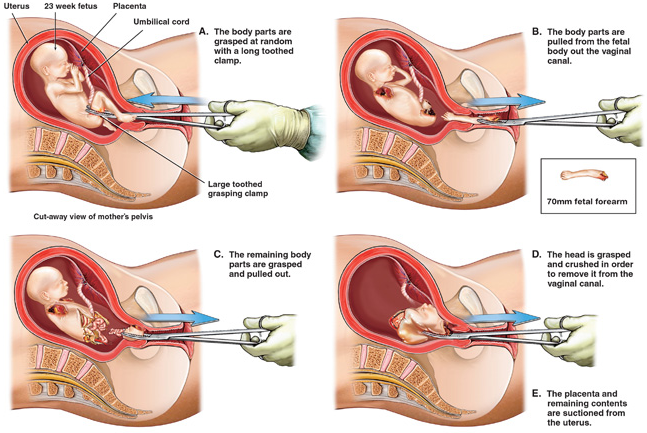 |
| Evacuation of the Uterus. Photo by SafeParentHood Malaysia |
Causes of Abortion
- Development defects such as a bicornuate uterus and myomas.
- Cervical incompetence.
- ABO incompatibility between mother and embryo may result in abortion.
- A retroverted uterus which is unable to rise out of the pelvis may occasionally predispose to abortion.
- Chromosomal abnormality or disease of the fertilized ovum may account for 60% of spontaneous, first trimester abortions.
- Malformation of the trophoblast and poor implantation of the blastocyst may result in placental separation with consequent hypoxia and impaired embryonic development.
- Disease: acquired during pregnancy such as rubella or influenza, especially if they are accompanied by acute fever, interfere with transplacental oxygenation and may precipitate abortion.
- Chronic disorder. For example renal disease accompanied by hypertension, may have a similar effect.
- Drugs: large doses of any drug are poisonous and should be avoided.
- Psychological factors.
Clinical Features and Treatment
Any woman of reproductive age with abnormal bleeding or pain should be considered to possibly have had an unrecognized pregnancy episode. Each new pregnant patient should also be instructed to notify her physician promply about vaginal bleeding or uterine cramps. Since management depends on a number of factors, let’s consider the clinical aspects of miscarriage under the following subgroups.
Threatened Miscarriage
Any bloody discharge or uterine bleeding that occurs during the first half of pregnancy has traditionally been assumed to be a threatened miscarriage. Because as many as 25% of pregnant women have some degree of spotting or bleeding during the early months of gestation, it is a common diagnosis.
Bleeding associated with threatened miscarriage is typically scanty, varies from a brownish discharge to bright red bleeding, and may occur repeatedly over the course of many days. It usually precedes uterine cramping or low backache. On pelvic examination, the cervix is closed and uneffaced, and no tissues has passed. The differential diagnosis includes ectopic pregnancy, molar pregnancy, vaginal ulcerations, cervicitis with bleeding, cervical erosions, polyps, carcinoma.
Although there is no convincing evidence that any treatment favorably influences the course of threatened miscarriage, a sympathetic attitude by the physician along with continuing support and follow-up are important to patients. If careful clinical evaluation indicates that the conceptus is no longer viable, the treatment options are expectant management and evacuation of the uterus.
Inevitable and Incomplete Miscarriage
A miscarriage is inevitable when bleeding or gross rupture of the membranes is accompanied by pain and dilatation of the cervix. The miscarriage is incomplete when the products of conception have partially passed from the uterine cavity, and protruding from the external os, or are in the vagina with persistent bleeding and cramping. Placental tissue is more likely to be retained when this occurs in the second trimester. Bleeding can be profuse and occasionally produces hypovolemia. A careful vaginal examination usually establishes the diagnosis. Evacuation of the uterus is advisable to prevent maternal vomplications from further hemorrhage or infection.
Complete Miscarriage
Patients followed for a threatened miscarriage are instructed to save all tissue passed, so it can be inspected. When the entire products of conception have passed, pain and bleeding soon ceases. If the diagnosis is certain, no further therapy is necessary. In questionable cases, ultrasound is useful to determine that the uterus is empty. In some circumstances, curettage may be necessary to be sure that the uterus is completely evacuated. Removal of remaining necrotic decidua decreases the incidence of bleeding and shortens the recovery time.
Missed Miscarriage
This is where expulsion of the conceptus does not occur despite prolonged period of embryonic death. The reason that some dead embryos do not abort spontaneously is not clear. Typically, the patient's symptoms of pregnancy regress, the pregnancy test becomes negative, and no fetal heart motion is detected by ultrasound.
Septic Miscarriage
Any type of spontaneous miscarriage can be complicated by infection. Septic abortion was once a leading cause of maternal mortality but has become less frequent primarily due to changes in abortion laws which has made pregnancy terminations by physicians available to women with unwanted pregnancies. The infection of septic miscarriages is most commonly endometritis but can progress to parametritis and peritonitis. These patients present fever, abdominal tenderness, and uterine pain. In severe cases, local infection progresses to septicemia and septic shock. Optimal therapy consists of evacuation of the uterus aggressive use of parenteral antibiotics before, during and after removal of necrotic tissue by curettage. Prompt removal of the infected tissue is important and should be performed within a few hours after beginning intravenous antibiotics.
Recurrent Miscarriage
Recurrent miscarriage (RM), traditionally defined as three or more consecutive first-trimester spontaneous losses, affects up to 1% of couples. Primary recurrent miscarriage is diagnosed in women who have never had a successful pregnancy and secondary recurrent miscarriage in those whose repetitive losses follow a live birth.
Known and Suspected Cause of Recurrent Miscarriage include;
- Stuctural uterine defects.
- Endocrine problems.
- Genetic Abnormalities.
- Autoimmune disorders such as Antiphospholipid Syndrome and Thrombophilic disorders.
- Cervical Incompetence.
- Idiopathic Causes, alloimmune factors have been suspected.
Read Also
Pregnancy Induced Hypertension (PIH)
Ectopic Pregnancy
Antepartum Haemorrhage
Postpartum Haemorrhage







0 Comments