INTRODUCTION
The essence of antenatal care is a thorough assessment at the first visit (history, examination, routine and indicated investigation) followed by assessments thereafter at appropriate intervals. This will reveal existing risk factors and any further deviations from normal at the earliest opportunity.
Risk factor analysis can be a complex and time consuming procedure since it may involve a wide range of factors. Major emphasis is placed on the preventive aspects of care – education and motivation of the woman, immediate medical care, referral for investigation or expert opinion, or an increase in the tempo of surveillance.
Proper antenatal management involves seeing the woman as early as practicable in the pregnancy, considerable care in obtaining all relevant information about the woman by history taking, examination and special investigation, thinking carefully about its obstetric significance and taking appropriate corrective action.
The meaning of the pregnancy to the mother and partner should be ascertained in terms of acceptance, preparedness and coping ability, any major stress, financial or other, should be determined. An overriding consideration of antenatal care is detection of the risk factors for both mother and baby, and reducing these to manageable and safe proportion by further investigation as indicated and matching risk to appropriate level.
In extreme case, this may involve the antenatal diagnosis of major foetal anomaly and termination of the pregnancy if thought to be necessary. The antenatal period is the ideal time to provide the mother with appropriate health education. E.g. diet, rest, exercise, breast feeding; the potential harm to the baby from alcohol and smoking should be indicated.
Antenatal care is a planned programmed of observation, education, and medical management of pregnant woman directed towards making pregnancy and delivery a safe and satisfying experience.
Women should attend ANC monthly up to 28 weeks then 2 weeks up to 36 weeks and then weekly 36 weeks thereafter.
High risk Mothers e.g. multiple pregnancies, suspected disproportion etc. should attend weekly.
THE FIRST VISIT: this is the particular routine through which the woman passes, it depends on variables such as private or public care and the size of the institution in the latter case.
INFORMATION TO OBTAIN DURING THE FIRST VISIT/ASSESSMENT
HISTORY
this involves taking information about the pregnant woman for the first time. The information should include:
- ADMINISTRATIVE DETAILS: these include the woman’s particulars such as name, place of abode, date of birth, occupation, next of kin, religion etc.
- FAMILY HISTORY: condition likely to be inherited by the woman such as diabetes, hypertension. Psychiatric disorders, twins, haemoglobinopathy etc.
- MEDICAL HISTORY: any of the following should be noted; allergies, cardiac disease, hypertension, renal diseases, central nervous disorders, psychoses, gastrointestinal or metabolic disease, blood transfusions rubella; any medications should be recorded.
- SURGICAL HISTORY: abdominal or pelvic operations in particular, as well as cardiac surgery and also injuries are recorded.
- SOCIAL HISTORY: relevant socioeconomic data are obtained, including information on the family adjustment and living conditions, and unusual stresses. Consumption of alcohol and drugs of addiction should be determined.
- GYNECOLOGICAL HISTORY: a history of venereal disease is important. Also previous disorders, such as abnormal cytology, infertility and gynecological surgery, are relevant.
- OBSTETRIC HISTORY: accurate details of all previous pregnancies must be obtained, including the year, period of gestation, duration of labour, nature of delivery and outcome, including sex and weight of the baby; also complication arising during pregnancy, labour and puerperium.
- PRESENT HISTORY: the history of the present pregnancy is obtained, which includes a careful review of all the systems. The date of last menstrual period should be noted, any contraceptive pill used, any infection she suffered; the woman diet during the pregnancy should be assessed etc.
SIGNIFICANCE/REASONS FOR ANTENATAL CARE
- To assist pregnant women to meet the nutritional status appropriate to their state.
- To identify any complication and find solution to it or to issue appropriate referrals.
- To educate them on public health issues such as malaria, hand washing after visiting the toilet, etc.
- To teach the women about labour, labour pains and what is expected during the labour process.
- To share information about what pregnancy is, how the baby grows and the need to take medication given at the antenatal care.
- To facilitate the woman and the family in preparation toward delivery.
SERVICES RENDERED AT THE ANTENATAL CARE
- Offering family planning services to couples and individual who need them.
- Provision of immunization to children.
- Offering counseling service to people.
- Rendering under five (5) clinics to mothers and their children.
- Treatment of minor ailment.
- Laboratory Investigations.
- Screening and treatment of STI.
GENERAL EXAMINATION
Three (3) techniques are employed here to examine the pregnant woman at the antenatal clinic. The examinations are carried out from head to toe of the woman. While going through the examination, you take note of any abnormalities that you may notice, so that appropriate measures can be put in place. The aspects considered include;
Inspection: This involves looking at the woman from the head to toe.
Her appearance
observe
the way she walk, any rashes on her body. Observe the breast for any abnormal
changes. Observe the vaginal for any soreness, warts and discharges. Observe
the mouth for sore, scent, swelling etc. Observe the extremities for edema
which may suggest PIH, any varicose veins on the legs, watch the colour of the
nails. Watch the abdomen to see whether it is pendulous or not. As it may give
clue that the woman may have contracted pelvis.
Palpation
this is
done on the abdomen. You palpate the abdomen to know the gestation age, the position
of the baby, any stretch marks on the abdomen, the fundal height, movement of
the foetus and the presentation.
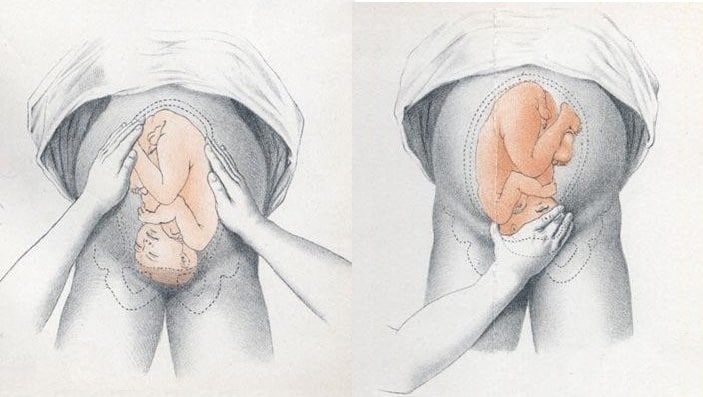 |
| Photo by teachmeobgyn.com |
Auscultation
PROCEDURE TO FOLLOW WHEN CONDUCTING ANTENATAL EXAMINATION
- First and for most, provide privacy and give reassurance to your client.
- Before examination, ask the woman to empty her bladder.
- Quickly inspect the woman from head to toe. Starting from the head, look at the colour of the hair. Look at the conjunctiva of the woman to rule out anaemia, inspect for signs of infection, swollen etc.
- From the mouth; watch the gums and examine the teeth, the colour of the mucosa membrane and refer if necessary.
- From the neck, watch for thyroid enlargement. Some enlargement is normal in pregnancy, but if this is associated with warm, moist hands, tachycardia and a jumpy woman, thyrotoxicosis should be considered and appropriate tests carried out.
- The breast should be inspected and palpated to determine the regularity of the breast, lumps and any flat or inverted nipple.
- Listen to the heart sound, the rate for any murmurs and carefully check the size of the heart which might indicate congenital, rheumatic or other disease. Also measure the blood pressure to rule out PIH.
- Assess the abdomen for any abnormalities such as enlargement of the liver, kidney or spleen.
- The vagina is examined for any infection (Candida, gonorrhea, trichomonas, etc.), abnormalities of the cervix (laceration, erosion etc.), and congenital anomalies such as double cervix and vagina or vagina septum. Condition predisposing to cervical incompetence should be carefully evaluated.
- The vulva should be examined for any varicose, previous tears and episiotomies, state of the perineal body and laxity of the introitus.
- The limbs are tested for oedema and the lower limbs for varicosities.
INVESTIGATION CARRIED OUT AT THE ANC/FIRST VISIT
- Weighing of the pregnant woman.
- Taking of the blood pressure to rule out eclampsia.
- Urine test to confirm pregnancy in certain cases.
- Blood test for Rhesus factor, haemoglobin, hepatitis B, HIV/AIDS, etc.
- Venereal disease test such as trichomonas, gonorrhea etc.
- Ultrasound test.
- Urine for diabetes, ketones, glucose etc.
Danger Signs during Pregnancy
- Vaginal bleeding
- Reduced fetal movement
- Frontal or recurring headaches
- Sudden swelling
- Rupture of the membranes
- Premature onset of contraction etc.
High Risk Factors in Pregnancy
- Domestic Violence.
- Smoking during pregnancy.
- History of multiple pregnancy.
- Exposure of mother to teratogens during pregnancy.
- Presence of maternal diabetes.
- Previous history of pre-term delivery.
- History of maternal hypertension or eclampsia.
- Presence of Sexually Transmitted Disease.
- Maternal Age.
BASIC PATIENT TEACHING CONSIDERATIONS FOR THE EXPECTANT MOTHER ON THE FIRST PRENATAL VISIT WITH REINFORCEMENT ON EACH SUBSEQUENT VISIT
- Instruct the patient on the importance of regularly scheduled follow-up visits (following the normal pregnancy).
- Once a month until the seventh month.
- Every two weeks during the seventh and eighth month.
- Weekly during the ninth month until delivery.
- Patient teaching must continue on each visit.
- Instruct the patient on the importance of proper nutrition.
- A well-nourished mother and baby are thought to be far less the victims of obstetric and prenatal complications, such as:
- Preeclampsia.
- Prematurity.
- Growth retardation.
- Significant residual neurologic damage (that is, cerebral palsy, mental deficiency, or behavior disorders in the child).
2. Guide to good diet from the six basic food groups daily.
- Milk, yogurt, and cheese group - 2 to 3 servings per day.
- Meat, poultry, fish, beans, eggs, and nuts group - 2 to 3 servings per day.
- Vegetable and fruits - 3 to 5 servings of vegetables and 2 to 4 servings of fruits per day.
- Breads, cereals, rice and pasta - 6 to 11 servings per day.
3. Proper weight gain for pregnancy. After an initial loss, the patient will gain 2 to 4 pounds during the first trimester. Expect a gain of a pound per week during the second and third trimesters.
 |
| The four basic food groups |
- Instruct the patient on the importance of proper rest and sleep.
- Pregnancy will cause the patient to tire more easily.
- Prevention of fatigue through short rest periods is vital to good health.
- The amount of rest or sleep required will vary with the individual and stage of her pregnancy.
- Instruct the patient on the importance of exercise and fresh air.
- The degree of exercise will vary according to her condition and stage of pregnancy.
- Walking is usually the exercise of choice.
- Swimming is an excellent overall exercise program.
- Instruct the patient on precautions to take during pregnancy.
- Decrease smoking or stop altogether if possible.
- Restrict or limit alcohol intake.
- Avoid children with measles or other contagious diseases
- Instruct the patient on potential danger signs of pregnancy that would necessitate her contacting her physician and visiting a health facility.
- Any vaginal bleeding, regardless of how small, may indicate miscarriage or abortion, placenta previa, or placenta abruption.
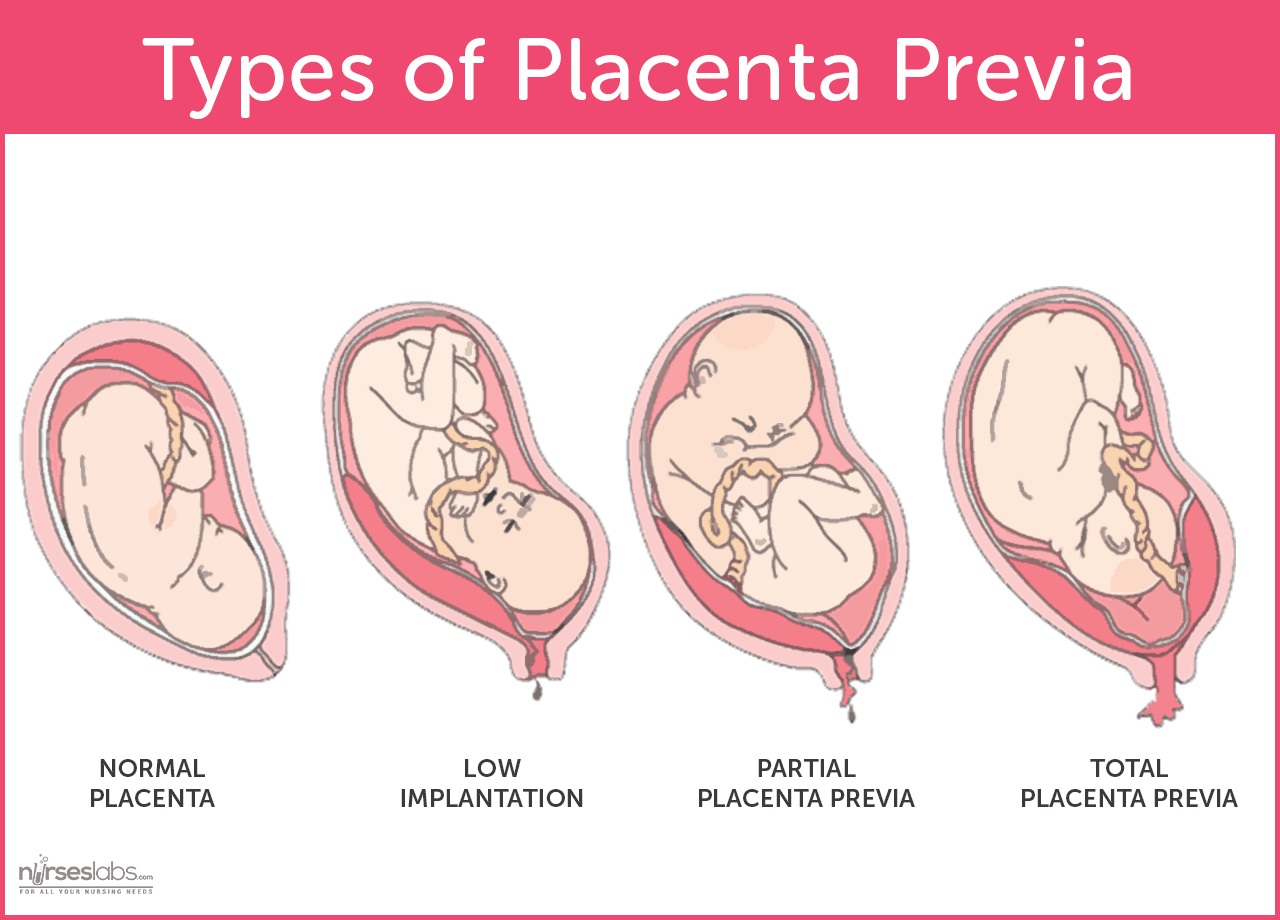 |
| Various
degrees of placenta previa. Photo by Nurseslabs |
 | |
| Various degrees of placenta abruption. Photo by SEIF & ASSOCIATES |
2. Symptoms that may indicate pre-eclampsia. The symptoms are:
- Severe continuous headache.
- Dimness or blurring of vision.
- Swelling of the face or hands, especially when present after resting all night.
- Scotoma - lashes of lights or dots before the eyes.
- Persistent vomiting.
- Sharp pain in the abdomen.
- Epigastric pain.
- Weight gain greater than 4 pounds in one week.
- Chills and fever.
- Burning upon urination.
- Sudden escape of fluid from the vagina. The patient should report immediately to the physician or the hospital. She should not wait for uterine contractions to start.
- Lack of fetal movement over a 24-hour period once "quickening" has been established.
- Regular uterine contractions less than 5 minutes apart for an hour for anyone less than 37 weeks pregnancy.








0 Comments