Introduction
Review of the Urinary System
 |
| Photo by Mount Nittany Health |
The urinary system includes the kidneys, ureters, urinary bladder and the urethra. The primary function of the urinary system is to maintain the body’s state of homeostasis by carefully regulating fluid and electrolytes, removing waste and providing hormones that are responsible for red blood cells (RBC’S) production, bone metabolism and the control of blood pressure. Superiorly to the kidneys we have the adrenal glands and inferiorly to the male urinary bladder you can find the prostate glands.
Urine is formed by the kidneys and flows through the other structures to be eliminated from the body. Microscopically each kidney has one million nephrons which allows for adequate renal function even if the opposite kidney is damaged or become non-functional.
The urine formed in the nephrons flows into the renal pelvis and then into the ureters that connect each kidney to the bladder and the urethra arises from the base of the bladders. The fluid is controlled mainly by the anti-diuretic hormone(ADH) released into the blood by the posterior pituitary gland which acts on the distal convoluted tubules and collecting ducts to maintain the fluid balance.
Urinary tract infections (UTI’S) are caused by pathogenic microorganisms in the urinary tract, the urinary tract is sterile above the urethra. UTI’S are classified into upper and lower urinary tract infections and can further be classified into uncomplicated or complicated depending on recurrent and duration.
Most uncomplicated UTIs are community acquired, common in young women and is not usually recurrent. Complicated UTIs, often nosocomial (acquired during hospitalization), normally occurs in people with urologic abnormalities or have recent catheterization. It is often recurrent.
Lower urinary tract infections include cystitis, prostitis and urethritis while Upper UTI’s include infections to the kidney and ureters such as Nephritis and pyelonephritis.
Risk Factors for UTI
- Inability/failure to empty bladder completely
- Immunosuppression
- Urinary tract instrumentation – catheterization
- Abrasion of the urethra mucosa
- Conditions such as diabetes, gout, pregnancy etc
- Obstruction in urinary blood flow due to:
- Urethral stricture
- Bladder tumours
- Calculi (stones in ureters or kidneys)
- Compression of ureters
- Contracture of bladder neck
- Congenital abnormalities
- Use of bedpan rather than commode or toilet
- Cognitive impairment
- Presence of infected pressure ulcers
- High incidence of multiple chronic conditions
- Immobility and incomplete emptying of bladder
Routes of Infection
Bacteria enters the urinary tract in 3 ways:
- By the transurethral route (ascending infection) – this is the most common route often from faecal contamination.
- Through the blood stream (haematogenous spread).
- Fistula from the intestine (direct extension).
Clinical Manifestations
- Burning on urination
- Frequency
- Urgency
- Nocturia
- Nausea
- Vomiting
- Loin tenderness
- Suprapubic tenderness
- Foul smelling urine
- Fever
- Incontinence
- Suprapubic or pelvic pain
- Haematuria
- Back pain
- Septic shock – in complicated UTI
Elderly patients often lack the typical symptoms of UTI and sepsis though frequency and urgency may occur. Nonspecific symptoms include:
- Lethargy
- Anorexia
- Low-grade fever
- Hyperventilation
- Altered sensorium may be the give a clue.
Diagnosis
- Urinalysis
- Mid-stream urine for urine culture and sensitivity – identify specific organism
- FBC
Management
Medical Management
Non-pharmacological treatment
- Liberal oral fluids to encourage good urinary output
- Personal hygiene and proper cleaning after defecation
Pharmacological treatment
Some medications used are:
- Ciprofloxacin or
- Co-amoxiclav or
- Cefuroxime or
- Gentamicin/ceftriaxone IV (in severe cases)
Nursing Management
- Assessment – history, symptoms, signs, sexual intercourse association, urine.
- Maintain patient privacy during examination and other procedures such as serving bedpan.
- Monitor and record vital signs, take appropriate intervention if required.
- Ensure adequate hydration.
- Monitor Intake and output.
- Temperature control.
- Pain assessment.
- Assist patient to assume a proper positioning, turn patient when necessary to avoid pressure ulcers which can further complicate patient condition.
- Serve medication as ordered.
- Obtaining appropriate urine and other samples for lab investigations
- Adequate nutrition
- Ensure perineal hygiene
- Patient education
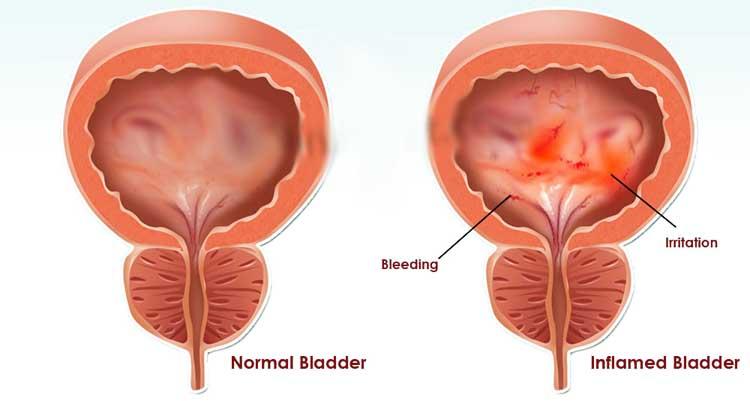
Cystitis
This is an inflammation of the urinary bladder.
 |
| Photo by Ask4Healthcare |
Causes of Cystisis
The infection is commonly due to gram-negative organisms; most frequently Escharichia coli (E. coli), other micro-organisms that cause lower urinary tract infections includes streptococcus, pseudomonas staphylococcus, gonococcus infections.
These infections results from faecal organisms that move from the perineum to the urethra and the bladder or spread through the blood stream to the urinary system. Also vesico-urethral reflux helps to transport the organisms.
Pathophysiology
For infection to occur, bacteria must gain access to the bladder and invade the epithelium to the urinary tract.
The organisms adhere to the mucosal surface and initiate the inflammatory process. Changes take place in the tissues such as redness, heat and hyperemia. Invasion of leukocytes and this brings about exudation and these changes initiates the signs and symptoms like fever, dysuria and others.
Renal Failure
Renal failure occurs when the Kidneys can’t remove body metabolic waste or perform their regulatory function.
The substance normally eliminated in the urinary accumulates in the body as a result of the impaired renal function, this leads to acid - base disturbances, fluid overload etc.
Renal failure is a systemic disease and can be acute or chronic.
Acute Renal Failure
Acute renal failure is a reversible clinical syndrome where there is a sudden and almost complete loss of kidney function over a period of hours to days.
Cause
Underlying causes are hypovolaemia, hypotension, heart failure and kidney stones. If this conditions are treated before the kidneys are damaged, the disease may be reversed.
Chronic Renal Failure
Chronic urinal failure is progressive, irreversible condition where the urinal function are impaired leading to uraemia or azotaemia. In this condition, there is complete destruction/damage of the nephrons.
Causes
- Diabetes mellitus
- Hypertension
- Pyelonephritis
- Untreated acute renal failure
Signs and Symptoms
- Oliguria
- Anuria
- Fluid retentions(oedema)
- Pulmonary oedema
- Anorexia
- Uraemia
- Hypertension
- Nausea/vomiting
Medical Management
- All medications must be given with caution
- Diet therapy
- Anti-hypetensive drugs e.g. atenolol, nifedipine
- Dialysis may be needed to reduce the uraemia
- Anaemia is treated with erythropoietine.gepogen
- Diuretics to see if patient respond by producing urine
Nursing Management
- Restrict all salt and potassium diet
- Monitor fluid intake (usually according to the daily loss)
- Monitor fluid and electrolyte balance
- Promote pulmonary function by nursing in upright position if there is pulmonary oedema. Assist patient to turn, and encourage patient to cough.
- Provide skin care
- Provide support
- Put measures to reduce metabolic rate e.g. bed rest
- Avoid nephrotoxic drugs and substance
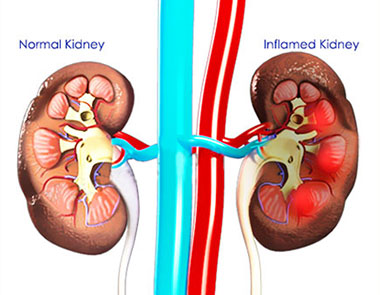
Nephritis
This is inflammation of the kidney especially the glomerulortubules and the renal tissue. It has been classified into Acute and chronic nephritis.
 |
| Photo by Planet Ayurveda |
Causes of Nephritis
It is caused by pathogenic microorganisms most often due to post streptococcal glomerulo-nephritis
Signs and Symptoms
- Oliguria
- Haematuria
- Fluid retention (oedema)
- Flank pain
- Fever
- Elevated jugular vein pressure (JVP)
- Increase blood pressure
Diagnostic investigation
- Urine analysis
- Urine culture
- Ultra sound scans (kidneys)
- Signs and symptoms
Management of nephritis
- To treat the streptococcal infections give oral penicillinVK500mg qid x 10 days or single dose of benzathinepencillin IM. If patients is allergic, give erythromycin 2. Give diuretics e.g. furosemide (lasix)
- Restrict fluid intake
- Restrict salt and potassium in diet
- Treat pressure areas if patient is having oedema
Risk Factors
- Kidney and bladder stone
- Diabetes mellitus
- Prostitutes
- CatheterizationImpaired voiding
- Pregnancy etc
Diagnosis
- Urine analysis
- Mid-stream urine specimen
- Ultra-sound scan of the bladder
- Clinical presentation
Clinical Features
- Dysuria
- Nocturia
- Urgency
- Frequency
- Burning sensation on urination
- Supra-pubic or pelvic pain
- Haematuria
- Pus in urine (pyuria)
Management
Medical management
- Antibiotic treatment should be started e.g ciprofloxacin ampicillin ceftriazone e.t.c
- Analgesics for pain
- Increase fluid intake
Nursing management
- Advice on the need to increase fluid intake
- Monitor intake and output and record
- Ask your patient to have frequency voiding
- Serve medication as ordered
- Educate sexually active women to have post coital voiding
- Monitor vital signs and record
- If necessary you pass a urethral catheter








0 Comments