Introduction
Personal Protective equipment (PPE) refer to specialized clothing or equipment worn by a health worker for the purposes of protection against infectious materials. It prevents direct contact with infectious agents or body fluids that may contain an infectious agent by creating a physical barrier between the potential infectious agent and the health worker.
Personal protective equipment (PPE) is used to protect both yourself and your parent from the risks of cross-infection. It may also be required for contact with hazardous chemicals and some pharmaceuticals. PPE includes items like gloves, aprons, masks, goggles or visors. In certain situations such as theatre, it may also include hats and footwear.
Risk assessment in the choice of a protective clothing:
- Nature of task to be performed.
- Degree of physical contact with the patient/client.
- Risk of contamination from blood or other body fluids.
- Whether there will be any contact with mucous membranes.
- Where sterile or non-sterile gloves are required.
- Barrier efficacy of the planned protective clothing/equipment.
- Client and latex sensitivity status.
Gloves
Gloves should be worn whenever there might be contact with blood and body fluids, mucous membranes or non-intact skin. They help protect you when directly handling potentially infectious material or contaminated surfaces. If gloves are to protect the wearer then non-sterile (clean) gloves will usually be appropriate, as they protect from heavy contamination during procedures and prevent staff-patient and patient-patient cross-infection. Gloves are not a substitute for hand washing: they provide a warm, moist environment that encourages bacteria to grow, and may be penetrated by external bacteria.
Furthermore, indiscriminate wearing of gloves may cause adverse reactions and skin sensitivity. Be sure, therefore, to wear gloves at the right time and for the right reasons. For example: gloves are not necessary when helping a patient onto a bedpan; to protect yourself from body fluids, however, wear gloves when removing a bedpan. Sterile gloves are necessary for invasive procedures and most procedures involving immunocompromised patients.
Remember therefore that hands are not clean merely because gloves are worn. Regular and effective hand washing is still essential before and after using gloves.
Gloves should be
worn:
- Only once, and should not be washed for reuse.
- When in contact with blood, body fluids or excreta.
- When handling soiled or contaminated equipment or linen.
- When caring for patients with a known infection, such as Methicillin-resistant Staphylococus aureus – MRSA, which is spread by touching another infected person.
Gloves should be
discarded:
- Between each patient, never wear the same pair of gloves for the care of more than one patient.
- If they become heavily soiled, or contaminated with infected material.
- If tom during patient care.
- Should be changed during patient care, if moving from a contaminated body site to a clean body site.
Types of Gloves
There are two types of gloves. Gloves, irrespective of the material used falls under the two; Nitrile or latex, polythene, neoprene, vinyl etc.- Clinical, that is, disposable (non - sterile or clean) gloves and surgical (sterile) gloves.
- Non-clinical/utility gloves; the plastic and leather.
Uses of gloves.
- They permit fine-motor movement when examining/carrying out a procedure on a client.
- When worn well, gloves protect the hands from contaminating and being contaminated.
- Generally, one can wear gloves when changing a soiled linen, washing bedpans, and dusting in the ward etc.
Precautions to remember when donning gloves.
- The hands are the common means of transmission of hospital acquired infection and the major area of blood contamination, thus gloves must fit correctly.
- Poorly fitting gloves can interfere with dexterity and performance, thus exposing the wearer to potential risks.
- Loss of tactile sensation could make needle stick injuries more likely to occur.
Donning and Doffing of gloves
Since disposal gloves are non - sterile, there is no strict laid down procedure for wearing them, surgical/ sterile gloves however require adherence to the instructions of the manufacture.
Donning Sterile Gloves
There are two methods for applying sterile gloves: open and closed. The open method is used most frequently when performing procedures that require the sterile technique such as dressing changes. The closed method is used when the nurse wears a sterile gown.
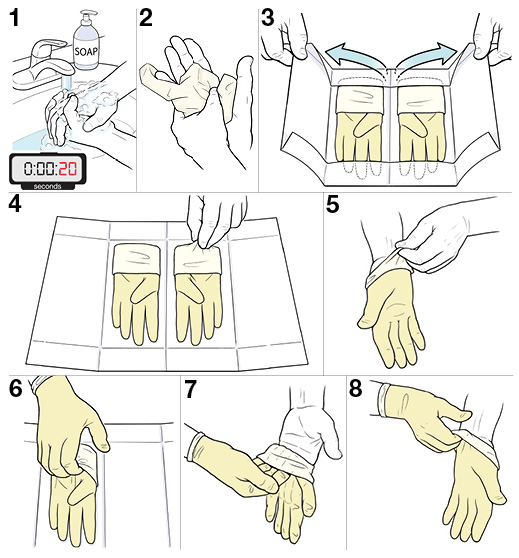
Performing open gloving and removal of soiled gloves
- Wash hands
- Read the manufacturer’s instructions on the package of sterile gloves; proceed as directed in removing the outer wrapper from the package, placing the inner wrapper onto a clean, dry surface (or a sterile surface if that what you are conducting a sterile procedure).
- Identify right and left hand; glove dominant hand first.
- Grasp the 2inch (5cm) wide cuff with the thumb and first two fingers of the nondominant hand, touching only the inside of the cuff.
- Gently pull the glove over the dominant hand, making sure the thumb and fingers fit into the proper spaces of the glove. [picture of gloving 1]
- With the gloved dominant hand, slip your fingers under the cuff of the other glove, gloved thumb abducted, making sure it does not touch any part on your nondominant hand. [picture of gloving 2]
- Gently slip the glove onto your nondominant hand, making sure the fingers slip into the proper spaces.
- With gloved hands, interlock fingers to fit the gloves onto each finger. If the gloves are soiled, remove by turning inside out as follows:
- Slip gloved fingers of the dominant hand under the cuff of the opposite hand or grasps the outer part of the glove at the wrist if there is no cuff. [picture of gloving 3]
- Pull the glove down to the fingers, exposing the thumb. [picture of gloving 4]
- Slip the uncovered thumb into the opposite glove at the wrist, allowing only the glove-covered fingers of the hand to touch the soiled glove.
- Pull the glove down over the dominant hand almost to the fingertips and slip the glove onto the other hand.
- With the dominant hand touching only the inside of the other glove, pull the glove over the dominant hand so that only the inside (clean surface) is exposed.
- Dispose of soiled gloves according to institutional policy and wash hands.
Aprons
These should be worn whenever there is a risk of contaminating clothing with blood and body fluids and when a patient has a known infection, for example, direct patient care, bed making or when decontaminating equipment. Discard or disinfect them as soon as the intended task is completed and then wash your hands.
They must be stored safely so that they don’t accumulate dust which can act as a reservoir for infection. Aprons are either plastic or cotton. Plastic aprons protect uniforms more effectively than cotton gowns which can easily get soaked with blood and other body fluids.
Description of the
apron
- Have hooks or ties that fasten around the neck.
- Have ties around the waist, reach around and tie at the back.
- Able to fit over the gown.
Aprons ensure that body fluids do not run into boots. It also prevents splash of body fluids on body clothing like the gown or uniform thus prevents staining the uniform.
Health professionals
recommended for wearing aprons:
- Nurses/midwives
- Laboratory technicians/staff
- Cleaning staff
- Corpse carriers
- Physicians, especially those who perform autopsies
Situations that require aprons
A clean apron should be worn and then discarded or disinfected afterwards when:
- Making Bed: ideally, patients known to be infected should have their beds changed last to reduce potential transmission of infection to vulnerable and uninfected patients; if linen is clearly contaminated with body fluids change the apron after handling.
- giving total patient care.
- assisting toileting.
- dispensing food and feeding patients - a special colour-coded apron may be worn for food handling.
- cleaning or performing other tasks likely to cause splashing and soiling of uniforms.
- involved with aseptic or invasive procedures.
Procedure for use
- Wash and dry hands.
- Select appropriate colour apron.
- Put apron over head, avoiding contact with your hair and uniform.
- Loosely secure apron at the back - this prevents splashes from trickling onto clothing.
- After procedure, break neck and waist ties by gently pulling apart.
- Fold inwards so that the potentially contaminated front does not touch hands or uniform.
- Discard into clinical waste bag or disinfect.
- Wash and dry hands.
Gowns
It is the outer layer of dressing worn over the scrub suit. It is worn in the theatre where surgical procedures are carried out. Impervious gowns or fluid resistant gown should be used when there is a risk of extensive contamination of blood or body fluids.
Description
- Open at the back, has ropes that can tie to close at the neck and at the waist.
- Should be at knee length.
- Should
have an elastic band to close the gown around the waist and wrist.
Usually worn by surgeons, surgeon assistants, scrub nurse and midwives in the labour room.
Masks, Visors and Eye Protection
These should be worn when a procedure is likely to cause blood and body fluids or substances to splash into the eyes, face or mouth. Masks may also be necessary if infection is spread by an airborne route. For example, multi drug resistant tuberculosis or severe acute respiratory syndrome (SARS). You should ensure that this equipment fits correctly, is handled as little as possible and changed between patients or operations. Masks should be discarded immediately after use.
Types of masks
- HIEPA (High Efficiency Particulate Air respirator).
- Filter or Biosafety mask.
- Dust-mist/cotton mask.
Criteria for donning all protective Clothing*
 |
| Photo by W.H.O |
The donning process of PPE should be done under the guidance and supervision of a colleague i.e. a trained observer.
- Remove all personal items such as jewelry, watches, cellphones, pens etc. in order not to risk infection.
- Put on scrub suit and rubber boots in the changing room.
- Move to the clean area at the entrance of the isolation unit and inspect (by visual) that the sizes of the PPE set are correct and the quality is appropriate.
- Perform hand hygiene, either by washing (preferable) or by using an alcohol based hand sanitizer.
- Don the first per of gloves (examination gloves).
- Put on disposable gown or outer gown.
- Put on face mask (nose mask).
- Put on face shield or Goggles.
- Put on head and neck cover.
- Put on disposable (plastic or rubber) apron.
- Put on second pair of gloves.
Criteria for doffing all protective clothing*
The criteria for removing protective clothing include disinfection with bleach solution and performing routine hand washing with soap and clean water, the hand hygiene in this case is done intermittently and is very important. Note that the highly contaminated clothing are; outer pair of gloves, apron, boots. While doffing PPE, make sure you don’t touch the front part of it because it is most likely the infected part. Perform this under the supervision of a colleague.
Follow the criteria
below;
Photo by W.H.O
- Perform hand hygiene; Wash gloved hands in soap and water and dip gloved hands into 1:10 bleach solution for one minute.
- Remove the apron leaning forward, if the apron is reusable, disinfect by spraying or wrapping it with 1:10 bleach solution.
- Perform hand hygiene on gloved hands and remove the outer pair of gloves.
- Remove head and neck covering taking care not to contaminate your face.
- Perform hand hygiene on gloved hands.
- Remove the gown by untying the knot first, the pulling from back to front rolling it from inside to outside and dispose of it safely.
- Perform hand hygiene on gloved hands.
- Remove the eye wear and mask from behind the head: wash eye wear with soap and water, place head cover in the laundry container, and hangs masks on hooks if reusable.
- Perform hand hygiene on gloved hands.
- Remove rubber boots without touching them. According to WHO, “appropriate decontamination of boots includes stepping into a footbath with 0.5% chlorine solution (and removing dirt with toilet brush if heavily soiled with mud and/or organic materials) and then wiping all sides with 0.5% chlorine solution. At least once a day boots should be disinfected by soaking in a 0.5% chlorine solution for 30 min, then rinsed and dried.”
- Remove the inner pair of gloves carefully. Avoid touching the front.
- Remove the inner wear of clothing (scrub suit).
- Wash hands with soap and clean water before leaving the theatre or changing room or isolation room.
* Some of the content were sourced from WHO.








0 Comments